The rapid increase of infectious disease cases and lack of adequate medical equipment to counter them can put the entire medical infrastructure at standstill. In times like these, it is up to engineers and technicians to come up with innovative solutions and provide extraordinary assistance.

Healthcare workers are very busy people who have to attend to the sick round the clock. And due to the widespread transmission of the highly contagious COVID-19 around the world, a record number of infected cases have been reported. This has made their job of improving a patient’s life strenuous. Adding to that, a general shortage of ventilation machines has put the entire medical infrastructure, including the support staff in a state of helplessness.
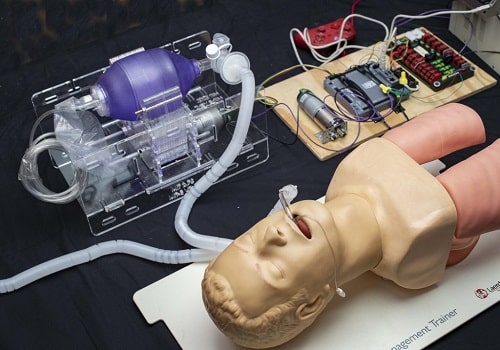
Several efforts have been made by various organisations and institutions across the globe to overcome this severe imbalance of demand and supply. One such cross-disciplinary team constituting of engineers, physicians, computer scientists and others from MIT has devised a ventilator that is highly efficient, portable and inexpensive.
Brief introduction about ventilator
When a person is hospitalised due to a respiratory illness (accompanied by shortness of breath), then that patient is put under a ventilator. It is a machine that provides mechanical ventilation, or artificially assisted air supply to support the patient’s respiratory organs such as lungs.
While a normal breathing rate is about 15 breaths a minute (BPM), an inability to respire properly can increase this rate to about 28 BPM. In such a scenario, a ventilator can play a crucial role in ensuring survivability.
Emergency ventilator
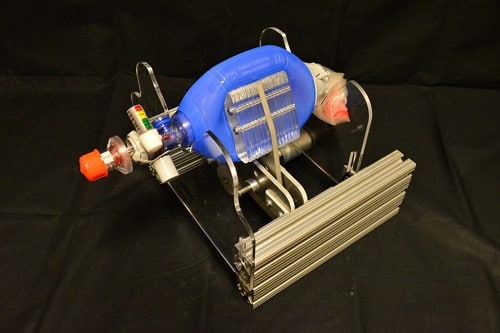
The inexpensive ventilator unit termed as MIT E-Vent (short for emergency ventilator) has been designed around a manual resuscitator, also known as an Ambu bag. This hand-held equipment is present in large quantities in several hospitals. With the help of manual compression, air is pumped into the lungs via the patient’s airway.
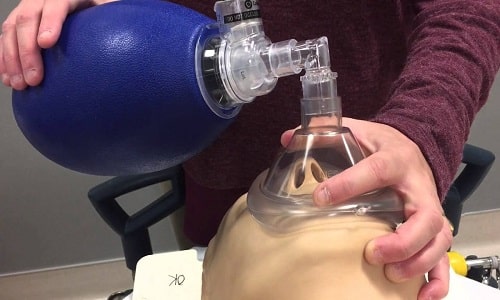
Since it was not possible to manually operate the Ambu bag for extended hours, the mechanically automated E-Vent was able to fulfil this purpose. Care was taken to not damage the bag and control its compression and decompression in such a way that the air pressure was suitably maintained according to the particular patient.
In case of any mechanical failure, the entire device could be immediately overtaken to function manually.
This design carries forward research that was previously undertaken at MIT. More about it can be read here.
Specifications
To adhere to strict safety guidelines, the team has laid down certain clinical specifications:
- Patients must be under the management of a trained clinician.
- The minimum controllable parameters to ventilate a patient should include:
- BPM (breaths per minute): between 8 – 40 BPM.
- Tidal Volume (TV) (air volume pushed into the lung): between 200 – 800 mL based on patient weight.
- I/E Ratio (inspiratory/expiration time ratio): recommended to start around 1:2; best if adjustable between a range of 1:1 – 1:4.
- Assist Detection pressure. When a patient tries to inspire, they can cause a dip on the order of 1 – 5 cm H2O, concerning positive end-expiratory pressure (PEEP) pressure (not necessarily equal to atmospheric pressure).
- Airway pressure must be monitored and:
- Maximum pressure should be limited to 40 cm H2O at any time; Plateau pressure should be limited to max 30 cm H2
- The use of a passive mechanical blow-off valve fixed at 40 cm H2O is strongly recommended.
- PEEP of 5-15 cm H2O required; many patients need 10-15 cmH2.
- Blending of oxygen and air-gas mixture to adjust FiO2 is not important in an emergency scenario. Ventilation on room air should also do.
- Covid-19 can get aerosolized (airborne), so HEPA filtration on the patient’s exhalation is required or between the ventilator unit and the patient (at the end of the endotracheal tube) to protect clinical staff from certain infection.
- Heat and moisture exchanger should be used in line with the breathing circuit.
- Failure conditions must result in an alarm.
As the above-stated project requires a specialized understanding of the clinical-technical interface, people with capable and adequate knowledge of medical technology are encouraged to design and further improvise it.
Open-source design
The team has released reference hardware design for meeting minimum clinical requirements, control strategies and electronics designs for safe ventilator functionality. It can be found here.
Despite the intensity of the work and the long hours, the team’s enthusiasm was never dulled as the primary consideration was patient safety and save lives that hung in balance.






thank you very much for the timely thought process, iff electricity available fine, if there is a power cut ,manual mode through foot operation can be thought off or may be useful at the peripheral health services.