Rapid progress in information technology and medical sciences has resulted in several implantable devices. This article focuses on the heart and related devices, which are used to provide cardiac resynchronisation therapy, help maintain rhythm, and prevent sudden cardiac death
The focus in personal healthcare has shifted from hospital care to home care and ultimately to healthcare on-the-move. As a result, the usage and popularity is rapidly shifting from fixed medical devices and systems to portable ones and ultimately to the wearable devices. The first-generation devices needed user involvement to obtain and record the data that was processed offline—for example, the heart holter used for monitoring and recording cardiac activity.
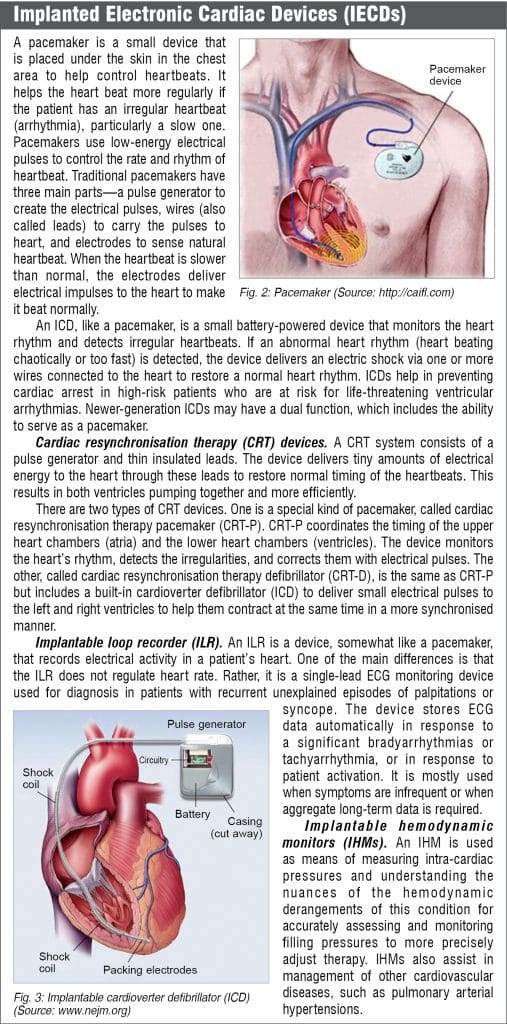
Rapid progress in information technology and medical sciences has resulted in several implantable devices. This article focuses on the heart and related devices. Implanted electronic cardiac devices (IECDs) include a broad spectrum of devices, such as pacemakers (PMs), implantable cardioverter defibrillators (ICDs), cardiac resynchronisation therapy (CRT) devices, implantable loop recorders (ILRs), and implantable hemodynamic monitors (IHMs). These devices are used to provide cardiac resynchronisation therapy, help maintain rhythm, and prevent sudden cardiac death (see box).

The heart of all these devices is a microprocessor with a miniature on-board power source. The microprocessor is programmed to collect data 24×7 and initiate the necessary action when it detects an event. For example, if the heart starts beating too fast, the device delivers a therapy to restore the normal heart rhythm.
The device, when implanted in a patient, needs regular monitoring. The patient has to make visits to the healthcare centre every three to six months to enable the healthcare team to check the device. During the visits, the data recorded by the device is downloaded to provide information regarding the significant events that have occurred, such as device malfunction, arrhythmia, changes in hemodynamic status or inadvertent changes in programmed parameters. This enables assessing the effects of the therapy as a part of a complete cardiac evaluation and optimisation of the device function.
 With increasing number of patients and the cardiac related problems, visits are becoming a heavy burden on healthcare systems. Remote monitoring communicates the information from the implanted device without the patient physically visiting the centre while the patient stays connected to the healthcare centre all the time. In remote monitoring, the data collected is synchronised and shared by the device with a transmitter located near the patient. The transmitter communicates the data online to a secure portal accessible by the healthcare team.
With increasing number of patients and the cardiac related problems, visits are becoming a heavy burden on healthcare systems. Remote monitoring communicates the information from the implanted device without the patient physically visiting the centre while the patient stays connected to the healthcare centre all the time. In remote monitoring, the data collected is synchronised and shared by the device with a transmitter located near the patient. The transmitter communicates the data online to a secure portal accessible by the healthcare team.
The evolution of remote monitoring technology
The first pacemaker was implanted in a human in 1958. The pacemaker did not last long but the patient lived to the age of 88 with as many as 26 pacemakers replaced one after the other in his lifetime. The modern era began in 1969 with the development of demand pacemakers, which generated a regular electrical pulse without variation on its own, on sensing that the heart was not beating regularly.

Initially, the pacemakers were able to pace only the ventricle. Next, the dual-chamber pacing, called physiologic pacing, was developed that could pace both the atrium and the ventricle. These pacemakers paced at a fixed rate without increasing the heart rate with the increased activity. The present-day ‘rate responsive pacemakers’ are able to increase the heart rate with increased activity.
Later, other implantable cardiovascular devices were developed to restore normal cardiac activation sequence and/or detect and treat a malignant arrhythmia. The need for remote monitoring was felt when the follow-up procedure became overwhelmingly resource-consuming and demanded differentiated human and technical resources. Moreover, the long distance between the pacing centres and the population agglomerates posed various problems.
Initially, Furman and his team transmitted data from a pacemaker through telephone connection using the trans-telephonic monitoring (TTM) method. The TTM device used was a 30-day looping event monitor, about the size of a pager that recorded and captured irregular heartbeats by constantly tracking the heart rhythm. The device provided a rudimentary evaluation of pacing and sensing function and the patient was still required to make in-clinic visits.

The modern, reliable, safe, and secure devices became viable in the 1970s with the availability of the advanced IECD technology, compact longer lasting batteries, microprocessors with fast speeds, and improved analysis techniques and interpretation algorithms. Biotronik was the first company to market a wireless remote home monitoring system that was FDA-approved. Later, other companies followed. Medtronic introduced CareLink in 2005, Boston Scientific brought out Latitude in 2006, and St. Jude started selling House Call in 2007.
Over the last few years, a number of advanced interpretation algorithms have emerged, improving the scope of analysis and diagnosis, and making the devices more and more complex.
How remote monitoring works
During the traditional follow-up visits to a health centre, a sensing wand is placed by the doctor over the device to download the data into a dedicated computer provided by the manufacturer. Analysing the data, the doctor learns retroactively the events that have happened, such as a high-energy shock or an abnormal activity of heart or the device. Remote monitoring makes possible the information available wirelessly without the patient visiting the centre.
The remote monitoring systems used earlier were non-wireless and transmitted the data when the patient placed a magnetic sensor over the device. The sensor fed the data into a phone modem to transmit it to the clinic or a remote monitoring service.
The present-day remote monitoring systems are wireless and automated. The data from an implanted device, which is compatible with the mostly proprietary remote monitoring system, is downloaded and shared automatically with a home monitor, located within three metres of the patient, using radio transmissions.

Some systems use a smart phone instead of the home monitoring device. The monitor dials up a phone based internet connection and transmits the data to a central server. The healthcare team accesses the data on their computer or a mobile device using a password-protected secure link. The system can transmit data at specific dates and times and/or can be set to transmit when triggered by the programmed alerts, such as the settings going out of range, delivered shocks, or abnormal heart rhythms.
The transmitted data includes such information as heart rhythm changes, device malfunctioning, fluid retention in the lungs, etc. The receiving devices are programmed to look for the specific alerts triggered by events and notify the information automatically to the doctor via a text message, fax, e-mail, or a website message. The information also gets downloaded into the patient’s electronic medical record (EMR).
Remote monitoring provides the healthcare team an easy access to information, enabling them to manage the patient’s heart condition and the function of the implanted device in a better and quicker way. The quality of life of patients is improved with reduced hospitalisation and curtailed visits to the clinics, and they also get a sense of security and peace of mind.
Electromagnetic and RF interference
Medical Implants Communication Services (MICS) frequency band, ranging from 402 to 405MHz, is available for use by implanted medical devices to provide high-speed communication between patients’ IECDs and medical practitioners. Choice of the frequency is made based on associated body losses and antenna efficiency. The 400MHz region offers optimisation in this respect with better ability to transmit radio signals in the human body.
However, IECDs are susceptible to electromagnetic interference (EMI) and radio frequency interference (RFI) when exposed to electromagnetic fields or radiations from radio transmitters. Potential sources include high-voltage transformers, powerful electromagnets, radio transmitters, and various types of electronic equipment and devices, such as mobile phones and antitheft devices.
The interference risk depends on factors such as distance from the source, transmitted power, and the level of protection provided in the device itself. The malfunctions of IECDs include over/under sensing, induction of asynchronous ventricular dysrhythmia, and electronic noise. As a safeguard, precautions are required to be taken by the patient, such as using cellular phone in the ipsilateral ear and maintaining distance from high-voltage transformers, machines, and gadgets/devices emitting strong electromagnetic radiations.
The systems available
Almost all the manufacturers are marketing proprietary IECDs that are compatible with their own remote monitoring systems and protocols only. As a result, collection and management of data requires manufacturer-specific equipment. Although there are operational differences, the general flow of information is similar. Some of the systems in use are:
Home monitoring. Biotronik, a German firm, was the first to introduce their remote home monitoring system in 2001. The system transmits data on a daily basis at fixed time intervals and on the occurrence of a clinically relevant event. A cell-phone-like patient device sends encrypted data automatically via mobile phone to a central database in Europe. On reception, the data is processed and made available to the caregiver.
Caretaker network. The CareLink network of Medtronic, USA, is one of the leading remote monitoring systems, which can be used by a compatible Medtronic patient implanted heart device. The system is customisable and flexible, and has a monitor that interfaces with the device and a telecommunications link to transmit data to the healthcare team.
CareLink also enables display of diabetes information, such as continuous glucose monitoring and insulin pump data. The network enables the healthcare team to access the information on a secure website or through a mobile app. Colour-coded notifications are made available to the patients via options that include website, voice message, pager, text message, or email message.
Lattitude. Pacemakers and defibrillators manufactured by Boston Scientific are available for use with their automatic latitude home monitoring system. However, they do not conduct continuous monitoring; they send the information automatically or prompt the patient to send it at the scheduled times. They can also monitor and send weight and blood pressure data to a secure website. The system delivers notifications at two levels—Red alerts and Yellow alerts. Security protocols are used to protect the medical information and only authorised people have access through a password.
Advantages of remote monitoring
The most significant benefit of remote monitoring is that it almost eliminates the routine visits to the doctor and substantially improves the survival rate of the patients. The system can detect in real time the cardiac events, abnormal heart rhythms, and any problems with the functioning of the implanted devices—allowing the healthcare team to respond faster.
Remote monitoring helps in reducing the volume of in-office patients, allowing healthcare team to attend to more patients. Hospitalisation need is reduced, improving the quality of life and allowing improved patient management by the heathcare team.
Studies carried out over a period of five years have shown that the people using home monitoring had a 50% relative risk reduction compared to the people making regular follow-up visits to the clinics. Also, in case of patients using implanted pacemakers and a smart device for remote monitoring, there was a significantly higher rate of scheduled transmission success compared with the traditional monitoring technologies.
It was observed that some people, especially, old and aged, found it cumbersome to set up the system on their own and needed technical assistance. Also, people travelling for a long period of time may find it inconvenient to carry the monitor with them.
Conclusion
Remote monitoring of cardiovascular implantable electronic devices was developed to complement the compulsory calendar based in-person evaluations and provide convenience to the patients as well as clinics. It has the potential to reshape monitoring of the patients as it substantially reduces the number of in-clinic visits without compromising patient safety, makes possible an early detection of clinically actionable events, and detects any malfunctioning of the implanted devices. Some systems can even connect with an ECG machine, a weighing scale, and a blood-pressure monitor.
The technology greatly assists the healthcare professionals in better managing the patients as well as the devices. Remote monitoring makes it possible to increase the number of patients that can be attended to without adding extra resources. Its use results in reduced expenses in follow-ups, possible admission, and treatment in a hospital, as well as the expenses incurred in consultation fees and transportation. There is time saving since travelling time is eliminated and there is no waiting period at the clinic for consultation.
IECDs compatible with Web based, remote monitoring systems are readily available in the market and almost all are proprietary in nature. The current technology does not allow remote reprogramming of devices, and the different proprietary systems remain a major obstacle to data integration. Ensuring the personal medical data security is another potential problem as the data is vulnerable to hacking.
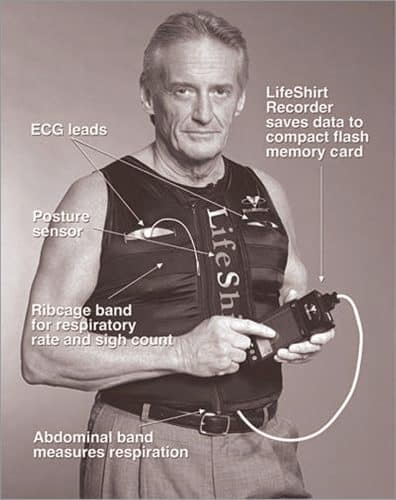
These issues are likely to be resolved with future technological developments. Vivometrics LifeShirt is a non-invasive ambulatory monitoring garment with embedded sensors, which is used to monitor up to 40 physiological parameters, such as heart rate, breathing, and lung capacity. Today’s devices have already far outpaced the capabilities of trans-telephonic monitoring and continuous development is taking place to enable them improve healthcare and at a lower cost.
Dr Deepak Halan is currently Associate Professor with Jaipuria Institute of Management, NOIDA